The feet are the first interface where the body connects to the ground. For patients with chronic diseases such as diabetes and gout, foot health not only affects daily walking and comfort, but is also closely related to the risk of complications and quality of life. In recent years, barefoot/minimalist shoes have gradually become a trend in Europe and America: they emphasize zero drop, wide toe caps and thin, flexible soles, aiming to restore the natural function of the feet. Can people with diabetes or gout wear barefoot shoes?
Why Foot Health Matters in Chronic Conditions
Diabetes: Long-term high blood sugar may lead to peripheral neuropathy (reduced or abnormal sensation in the feet) and vascular disease (poor peripheral circulation). Therefore, even minor friction, cuts or blisters may develop into ulcers or infections that are difficult to heal, and in severe cases, may result in amputation.
Gout: The metatarsophalangeal joint of the big toe is most commonly affected. During acute attacks, the joint experiences severe pain, redness and swelling. Chronic hyperuricemia may cause joint deformity and abnormal weight-bearing.
Therefore, any external factors that affect the force on the feet, the integrity of the skin or blood supply – such as shoes – must be carefully selected and monitored.
What Are Barefoot Shoes? Key Design Features & Biomechanics
Common features of barefoot/minimalist shoes:
Zero drop: No height difference between heel and forefoot, promoting a more natural stance.
Wide toe box: Allows toes to splay and engage during gait.
Thin, flexible sole: Enhances ground sensory feedback (proprioception), encouraging foot muscle activation.
Minimal arch support: Encourages the foot’s intrinsic structures to bear load.
Biomechanically, barefoot shoes can restore sensory feedback and activate intrinsic foot muscles, potentially improving gait and posture. But thinner soles also mean less physical protection from sharp objects, heat, and other hazards, which is especially relevant for at-risk feet.
Diabetes: Benefits, Risks and Practical Considerations
Possible benefits
Enhancing proprioception and balance: For patients with acceptable sensation, a thin floor can restore some ground perception and may reduce the risk of falls.
Improving the lower limb power chain: Activating the muscles around the toes and arches of the feet may help relieve knee/hip pain caused by misalignment or poor gait in the long term.
Reduce local compression of the front foot: A wide toe box helps prevent skin damage caused by hallux valgus or friction between the toes.
Main risks
Painless injury caused by sensory loss: If patients have moderate to severe peripheral neuropathy (dullness/loss of sensation), they may not be able to notice in time the friction inside shoes, blisters or punctured soles of the feet.
Poor blood supply leads to slow healing: The same minor trauma heals more slowly in diabetic patients and has a higher risk of infection.
Improper transition can cause fatigue damage: Wearing thin-soled shoes for a long time without training the foot muscles may lead to overloading of tendons/muscles (such as pain in the tibialis anterior muscle or plantar fascia).
Recommendations for people with diabetes
First, consult a professional doctor or podiatrist: especially for those with a history of ulcers, significant loss of sensation or peripheral artery disease (PAD), it is often contraindicated or extremely cautious.
Graded try-on: Start with a short period indoors (for example: 10 to 15 minutes per day), walk on a flat and safe ground first, and then gradually increase the time and intensity of the activity.
Daily foot examination: Every day, use a mirror or someone else to check the soles of your feet, between your toes and on your heels for any red spots, blisters or cracks.
Choose barefoot shoes with a certain degree of coverage but not overly thin soles: Compared to completely “barefoot imitation” toe clamping and sandal designs, prefer closed barefoot shoes with good coverage, smooth stitching, and soft materials.
Use seamless diabetes socks with fitted insoles (if necessary) : This can reduce friction and increase cushioning in certain areas.
If any discomfort occurs, stop immediately and seek medical attention.
Gout: Considerations for Barefoot Shoe Use
Possible benefits
Wide toe box reduces pressure: Gout often affects the big toes. A wide toe box can reduce mechanical irritation and friction, enhancing comfort during non-attack periods.
More uniform force line distribution: The zero-drop design can help adjust the center of gravity on some individuals and reduce local high pressure on the forefoot or metatarsophalangeal.
Risks and Limitations
Obvious discomfort during acute attack: During the acute stage of gout, avoid wearing any shoes that may touch or press the affected area. Prioritize rest, ice application and medication control.
For those with severe deformation, custom-made support or cushioning is required: If the joints are significantly deformed or accompanied by abnormal gait, barefoot shoes alone may not be sufficient to provide the necessary cushioning or correction.
Recommendations for people with gout
During the acute stage, wearing thin-soled barefoot shoes is prohibited. Wait until the redness, swelling and pain subside before making an assessment.
When choosing styles, pay attention to the toe space and soft upper. If necessary, use detachable insoles to add local cushioning.
Gradually adapt and record the changes in symptoms: If the big toe or metatarsophalangeal toe remains uncomfortable after wearing, stop using it immediately and consult a doctor.

Real-World Experience
Note: The following summaries are drawn from publicly available user reports, community discussions, and brand reviews — they are individual accounts (not randomized clinical trials) and should be treated as anecdotal evidence.
U.S. media interview / diabetic user (example): A diabetic individual without active ulcers tried barefoot shoes with physician approval. Starting indoors for short durations, they reported increased activation of foot muscles, better balance, and reduced knee discomfort—while emphasizing daily foot checks and gradual progression.
Evidence type: Media interview / user self-report.
UK diabetes community discussions: Members on diabetes forums have mixed views. Some report positive outcomes after cautious trial; others warn that those with sensory loss or ulcer history should avoid minimalist options.
Evidence type: Community forum discussions.
Reddit and social groups: Individuals with mild neuropathy say they benefit from barefoot shoes when used indoors or on smooth surfaces; however, reports exist of users developing blisters after neglecting regular foot inspection.
Evidence type: Social media posts / anecdotal experiences.
Brand reviews — gout sufferers: Several purchasers with gout praise the wide toe box and comfort in non-acute phases, but note no relief during attacks.
Evidence type: Customer reviews.
Summary: These accounts show that under medical supervision, careful adaptation, and strict monitoring, some people with diabetes or gout have successfully used barefoot shoes. But the approach must be highly individualized.
A Safe Starter Plan (Step-by-step)
Medical assessment: First, consult the attending physician, endocrinologist or podiatrist to assess whether there is a history of foot ulcers, loss of sensation, severe vascular disease or other contraindications.
Principles for choosing shoes
1️⃣Closed upper (preferred) > slipper/sandal style.
2️⃣Wide toe, no inner seam irritation points, and soft upper.
3️⃣The sole does not have to be extremely thin (a thin cushioning layer can be selected initially to ensure protection).
Adaptation period plan (Example) :
Monday to Tuesday: Stand and walk indoors for 10 to 15 minutes each time.
From Wednesday to Thursday: Extend to 30 minutes each day and try short walks on flat ground.
Week 5-8: Gradually increase to 1 hour per day (depending on the reaction of the feet).
If redness, swelling, blisters, stinging or numbness worsen at any time, stop and seek medical attention.
Nursing and Monitoring
Check the soles of your feet and the Spaces between your toes every day. Use a mirror or ask your family for help.
Keep the skin clean and moisturized (but avoid moisture and fluid accumulation between the toes).
If there is a small wound, disinfect it as soon as possible and seek medical assessment.
FAQ
Q: Can all people with diabetes wear barefoot shoes?
A: No. Those with severe neuropathy, active ulcers, or significant PAD are generally not candidates. Mild cases may try under medical guidance.
Q: What about gout attacks—can barefoot shoes help?
A: Not during acute attacks. They may help with comfort in the intercritical (non-acute) periods if adequately roomy.
Q: How to choose my first minimalist pair?
A: Look for closed, supportive minimalist shoes with a wide toe box and minimal internal seams. Avoid sandals and very thin prototype soles at first.
Conclusion & Practical Takeaway
Barefoot shoes are neither an automatic “no” nor a magic solution for people with diabetes or gout. For selected individuals without active foot disease and with clinician approval, they can serve as a complementary tool to enhance proprioception, strengthen foot muscles, and potentially improve gait mechanics. The guiding principles are medical clearance, a cautious graded transition, daily self-monitoring, and stopping immediately if any adverse signs appear.
Disclaimer & Contact
This article is educational and not medical advice. Consult your healthcare provider or podiatrist before changing footwear strategies, especially if you have diabetes, gout, peripheral neuropathy, or vascular disease.
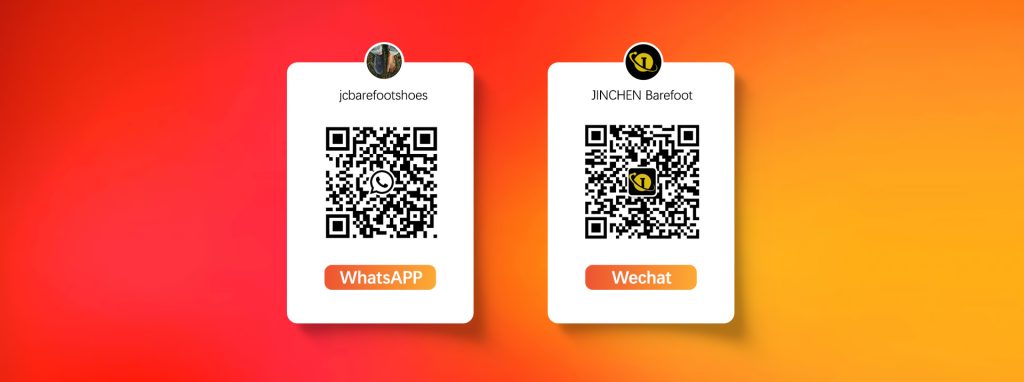
For personalized advice or recommendations for barefoot shoe models suited to specific foot conditions, contact our health advisory team:
Email: barefoot@jinchenshoes.com
Phone: +86 199 3076 5088